This information is for you if you have been offered hysteroscopy as an outpatient. It may also be helpful if you are a partner, relative or friend of someone who has been offered this procedure.
What is a hysteroscopy and how is it done?
Outpatient hysteroscopy is considered to be the best way to examine the uterus (womb) as they are quick, successful, safe and can be done without the use of a general anaesthetic (being asleep).
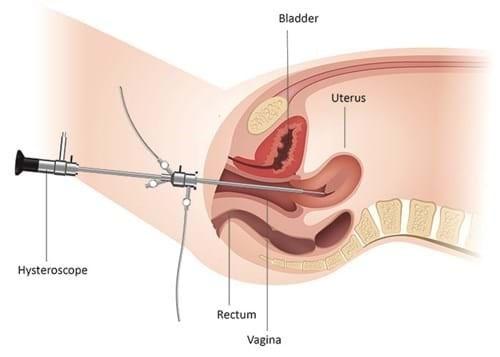
Hysteroscopy is a procedure that allows the inside of your uterus (womb) to be examined to diagnose and treat causes of abnormal bleeding or reproductive problems without having to operate (cut your skin). Anything outside of your uterus, such as ovaries, cannot be seen during this procedure. A hysteroscope is passed through your vagina and through your cervix (neck of the womb).
The hysteroscope is very thin, less than 4mm wide, and has a small camera and a light to see the inside of your uterus. This image can be seen on a screen by both your healthcare professional and yourself, if you choose to look.
Why have I been referred for a hysteroscopy?
There are a number of reasons why you may have been referred for an outpatient hysteroscopy, including:
- post-menopausal bleeding or irregular bleeding whilst you are taking hormone replacement therapy (HRT)
- bleeding between your periods or bleeding after sex that affects your quality of life, that medication does not help
- if you are thinking about having endometrial ablation (a procedure to make your periods less heavy)
- investigating something that has been found on another scan, such as a suspected uterine polyp on an ultrasound scan
- in vitro fertilisation (IVF) or recurrent miscarriage investigation
- finding and removing a lost coil
- looking for uterine synechiae (scar tissue in your womb)
Are there any reasons why I shouldn't have hysteroscopy as an outpatient?
There aren’t many reasons why we would not perform an outpatient hysteroscopy. They include:
- previous surgery to remove your uterus and cervix
- if you have been a victim of female genital mutilation (FGM) we may not be able to perform this procedure in the outpatient setting
- if you are pregnant we cannot perform the procedure due to the risk of causing a miscarriage
- unpleasant smelling discharge, pelvic infections or active genital herpes will mean that the procedure will have to be postponed to reduce the risk of further infection
- if you have found a previous hysteroscopy very painful, find cervical smears very difficult or painful, faint due to period pain or have had severe pain during a previous vaginal examination, an outpatient hysteroscopy may be difficult for you to tolerate
- being on certain medications, particularly anticoagulants (blood thinners)
These will all have been discussed with you and your doctor before arranging the hysteroscopy as an outpatient.
What are the potential risks?
As with any procedure, there are risks that you need to be aware of. These risks will be discussed further at your appointment. The risks are reduced by having the procedure as an outpatient.
Very common risks (1 in 1 to 1 in 10 people)
Pain: This procedure can be uncomfortable both during and for a short time afterwards. Everyone’s experience of this pain is different. The pain is usually described as similar to a period cramp low down in your abdomen (tummy).
Bleeding: You may experience some bleeding both during and after the procedure. We expect a small amount of bleeding and consider this to be normal due to what happens in the procedure, and will settle.
If you keep bleeding or there is a lot of blood we would consider this not normal. We may need to help you with treatment depending on the cause of the bleeding so please contact Greenoaks or B11 to let us know if this is happening.
If you take anticoagulants (blood thinners) or have a bleeding disorder, you will need to have had an international normalised ratio (INR) blood test at least 1 week before your appointment with a result of less than 3. If the result is above 3, please contact your General Practitioner (GP) and inform the Contact Centre on 01709 427676 as your appointment will need to be rescheduled until the level is correct. Do not stop taking your medication.
Common risks (1 in 10 to 1 in 100 people)
Vasovagal syndrome (blood pressure dropping causing you to faint), fainting or feeling sick: Moving or dilating (opening) your cervix can result in a low heart rate and a drop in blood pressure, causing you to faint or feel nauseous (feel sick). This is due to stimulating the vagal nerve and happens to less than 1 person in every 10 procedures. This can happen whether local anaesthetic (numbing the area) has been used or not.
Rare risks (1 in 1000 to 1 in 10000 people)
Infection: The risk of infection after an outpatient hysteroscopy is very low, around 1 in 1000, due to the procedure being sterile (totally clean). As such, we do not routinely prescribe antibiotics. If you do get an infection, you may need antibiotics from your GP. Signs and symptoms of this are:
- heavy vaginal discharge or bleeding
- a raised temperature
- lower abdominal (tummy) or back pains
Uterine perforation: The risk of this procedure causing a tear in your uterus is less than 1 person in every 1000 procedures. In the rare circumstances of this happening you may need to stay in hospital overnight for observations and antibiotics or a diagnostic laparoscopy if needed.
How should I prepare for my hysteroscopy?
Before coming to the clinic for your procedure, please:
- use contraception for at least 14 days before your appointment. You should ensure that there is no chance of you being pregnant when you have your hysteroscopy. On the day of the procedure you will be asked for a urine sample to perform a pregnancy test if you are age 55 or under. Your procedure will be rescheduled if there is a possibility that you might be pregnant.
- eat and drink normally. There is no reason to starve as you are not having a general anaesthetic (asleep). It may make you less likely to feel faint or nauseous throughout the procedure.
- allow plenty of time to get to your appointment to help alleviate traffic and parking related stress.
- take your usual medications, unless discussed beforehand.
- take your usual pain relief (paracetamol and ibuprofen) 1 hour before your appointment.
- wear loose or comfortable clothing to your appointment. Sheets will be provided for modesty in all instances.
You don’t have to bring someone with you, but it may be helpful to have someone you are comfortable with to support you.
If you need an interpreter or information about your care in a different language or format, please let us know so this can be arranged.
About intimate examinations
The nature of gynaecological care means that intimate examinations are often necessary. We understand that for some people, particularly those who may have anxiety or who have experienced trauma, physical or sexual abuse, these examinations can be very difficult.
If you feel uncomfortable, anxious or distressed at any time before, during, or after an examination, please let your healthcare professionals know. If you find this difficult to talk about, you may communicate your feelings in writing. Your healthcare professionals are there to help and they can offer alternative options and support for you.
Remember that you can always ask them to stop at any time and that you will have a chaperone to present. You can also bring a friend or relative.
What will happen at my appointment?
The appointment will begin with a consultation with the Hysteroscopist in the procedure room. It is a large, theatre like room which has all the equipment needed to perform your hysteroscopy.
There will also be a nurse and a support worker present during the appointment.
The consultation will include discussion around:
- a history of your current complaint including the impact this has on your quality of life
- the date of your last menstrual period or when you went through the menopause
- any medical problems or past surgeries including any previous treatments to your cervix
- any pregnancies you may have had, including miscarriages and terminations
- the type of delivery of any children you have had
- a list of medications you take and any allergies
- most recent international normalised ratio (INR) blood test results if applicable
- whether you are up to date with your cervical screenings and if they were all clear
- the results of any other scans or blood tests you may have had prior to the procedure
- a consent form will be filled in and signed by both yourself and the Hysteroscopist.
You may find it helpful to write some of your answers down in preparation for your appointment, or any questions you have.
What happens during the procedure?
You will be shown where to remove your clothing and a sheet will be provided to maintain your dignity. You can leave your socks on if you wish. You will be helped onto the couch and have your legs in stirrups and the couch will be raised.
To help us to see inside your uterus we use lots of sterile fluid which may be cold. This will trickle back out and may feel strange.
We do not always use a speculum but it may be required in some cases. This will be discussed with you at the time.
The Hysteroscopist will look inside your uterus and may take pictures to be stored in your medical notes. The screen used by the Hysteroscopist to see inside can be seen by you too, if you want to watch, but you do not have to.
It is important for you to let us know if you feel pain that becomes too much so that we can stop the procedure.
Once the procedure is finished, the couch will be lowered and you will be asked to slowly sit up before getting dressed.
What might be found?
During the procedure we may find a number of things to suggest a cause for the problems you are experiencing such as:
- thickened endometrium (lining of the womb)
- polyps (small growth, most often these are not cancerous)
- fibroids (non-cancerous growth, which can range in size)
- abnormal structures such as a bicornuate uterus (‘heart’ shaped uterus)
Any findings will be discussed with you before leaving the room.
What other procedures can you do?
If we see any of the above, we may be able to ‘see and treat’ by performing extra procedures within the same appointment. This will always be discussed with you before doing and may include:
- biopsy - Small piece of tissue removed from a polyp or fibroid to send to the laboratory for more information.
- endometrial sample or endometrial biopsy - Taking a sample from the lining of your uterus using either the hysteroscope or after inserting a speculum and passing a thin tube through your cervix. This is then sent to the laboratory for further information.
- polyp removal / Versapoint - Using heat to detach polyps which can then be removed from the body and sent to the laboratory for further information.
- Hormonal coil or intrauterine system removal/insertion - the risks and benefits of this will be discussed with you before any insertion. It can take up to 6 months for the hormonal coil or intrauterine system to settle and for you to see any improvement.
Some other procedures we offer may need a separate appointment. These options include:
- fibroid resection / MyoSure - Fibroids affect around 15 in 100 patients. Small fibroids are easily removed in the outpatient setting, and is successful in 7 to 8 out of 10 patients.
- endometrial ablation / NovaSure - This is a minimally invasive procedure. It is only an option for people who have completed their biological families.
What will happen after the procedure?
Following the procedure you will be escorted to our recovery area where you will stay for around 20 minutes and refreshments will be offered. You may stay longer if needed.
You will need to wear a sanitary towel as you may have some bleeding following the procedure. The sterile fluid used throughout the procedure will also leak. Do not use tampons or menstrual cups for 1 week following the procedure as these may cause an infection.
You may have some cramping, this will reduce throughout the day. If required, take your usual painkillers. It is advisable to take the rest of the day to allow your body time to recover. After this time if you still feel like you need time to recover, rest as needed.
Normal physical activity and sex can be resumed when any bleeding and discomfort has settled. You can shower as normal but we advise no baths or swimming for 1 week following the procedure.
If you have been prescribed any other medications, these will need to be collected from our in house pharmacy before leaving.
If further blood tests or scans are required, you will be told how you can arrange these.
What do I do if I feel unwell?
If you experience any of these symptoms:
- heavy vaginal discharge or bleeding
- a raised temperature
- lower abdominal (tummy) or back pains
please contact Greenoaks Gynaecology Clinic on 01709 427641, 8:30am to 5pm, Monday to Thursday and 8:30am to 1pm on Friday. Outside of these times please contact B11 (gynaecology ward) on 01709 424349 who are available 24 hours a day.
Frequently asked questions
Is a hysteroscopy painful?
The procedure can be uncomfortable but it is difficult to say how much pain you would feel as everyone is different. It tends to be a low down period type cramp which is caused by your cervix being stretched and the pressure from the fluid we use to inflate the uterus to help us to see. The pain does not usually last very long and resolves between a few minutes and a few hours after the procedure.
If you find the procedure too uncomfortable, tell the doctor or nurse, they can stop the procedure at any time. If you are worried, speak to the doctor or nurse before having the procedure about what to expect and ask them about pain relief options.
Why is fluid used?
We use sterile saline to open up the inside of your uterus so that we can see the whole of the uterine lining and also allows outpatient diagnostic hysteroscopy to be completed quickly. If polyp removal is needed, the fluid also allows us to utilise the Versapoint (see earlier in the information).
How long does the procedure take?
The actual procedure takes around 10 to 15 minutes. This will be longer if performing any additional procedures. The full appointment time will be longer due to the pre procedure checks, consultation and recovery time.
What if I am unwell or unable to attend?
If you are unwell, including flu or COVID symptoms or are unable to attend your appointment for another reason, please get in touch with the Contact Centre to reschedule on 01709 427676 available Monday to Friday, 8am to 6pm.
Can I still have an outpatient hysteroscopy if I'm bleeding or on my period?
It is best to keep the appointment. Sometimes it can be difficult to do the test if you are bleeding heavily. Please contact Greenoaks if you have any concerns.
Do I need to use contraception?
The procedure cannot be performed if there is any chance that you are pregnant.
To avoid this possibility, it is important to use contraception or avoid sex between your last period and your appointment. This also applies if you are undergoing fertility investigations.
We will ask everyone up to the age of 55 to produce a urine sample and take a pregnancy test before the procedure.
Do I need to shave?
If it makes you feel more comfortable then you may, but this is not at all necessary.
What happens if the procedure is not successful?
If the hysteroscopy cannot be completed, which may happen for a number of reasons, your Hysteroscopist will discuss other options with you.
It may be beneficial to attempt the hysteroscopy in an operating theatre, usually as a day case, so we can ensure your complaint is fully investigated, and any potential treatments can be given. The benefits of this will outweigh the risks associated with general anaesthetic.
How long will it be before I find out the results?
Your doctor or nurse will discuss their findings with you before you leave, although it may take 2 to 6 weeks to get the results of a biopsy.
Your GP will be informed about the outcome of the procedure.
How will I get my results?
You will either receive a letter or a further appointment. You will be informed of which at the time of your procedure.
Can I drive after having a hysteroscopy?
This is entirely dependent on how you feel. You may have had some stronger pain relief during your procedure and we would advise you to stay in our recovery area for a little longer if you are driving yourself home to ensure it is fully out of your system.
When can I return to work?
You will be able to return to work the next day. However if the bleeding is heavy and you are concerned, please see your GP.
Can I travel?
Although there are no known health grounds for avoiding travel following a hysteroscopy, overseas medical attention for complications arising from treatment may not be covered by insurance. It is always best to check with your holiday insurance provider.
If you are going on any holidays or spa days involving swimming or spending time in a hot tub, it might be best to postpone the procedure due to the infection risk.
Will the procedure affect my period?
Your period may start earlier than usual, and may also be heavier.
What do I do if the bleeding happens again?
This will be discussed with your Hysteroscopist on the day. Each individual case may have different advice regarding this.
How to contact us
Greenoaks Gynaecology Clinic
01709 427641
8:30am to 5pm, Monday to Thursday
8:30am to 1pm on Friday
B11 (gynaecology ward) and the Acute Gynaecology Unit
01709 424349
Available 24 hours a day
