Having a pacemaker fitted
This information is for people who are having a pacemaker device fitted.
Cardiology
What is a pacemaker?
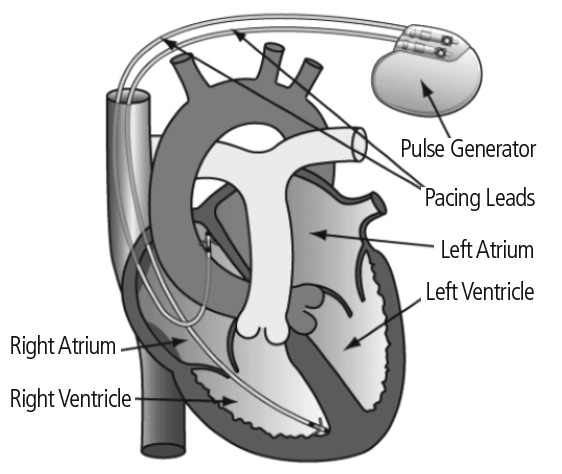
A pacemaker is a small electronic device which is used to treat some abnormal heart rhythms which can cause your heart to beat too slowly or miss beats. Some pacemakers can also help the chambers of the heart beat in time.
The pacemaker is fitted under your skin and 1 or 2 leads are positioned within the chamber(s) of your heart. The pacemaker is smaller than a matchbox in size and is only half a centimetre thick.
The pacemaker contains a power supply (or battery), which will need replacing after 8 to 10 years, depending on individual patient needs.
How does a pacemaker work?
A pacemaker checks your heart rhythm all the time. A normal healthy heart beats around 50 to 100 times per minute. If the pacemaker senses that you have an abnormally slow heartbeat or a series of missed beats, it will send electrical signals to your heart to make it beat normally.
The hospital will set up your pacemaker in the best way for the heart condition your doctor is treating you for. A fixed rate pacemaker works all the time, but most pacemakers are set to work on demand. That means they only work when they need to.
If you pacemaker needs to be reprogrammed after it has been put in, this is usually done in the pacemaker clinic.
Why do I need a pacemaker?
You may need to have a pacemaker if:
- your heart's natural pacemaker isn't working properly
- the natural electrical activity of your heart is slower than it should be
- you are fainting, having falls or feeling dizzy, tired or confused because of a very slow heartbeat
- the lower parts of your heart are beating out of time.
Different types of pacemaker
Your heart has four chambers. The top chambers are called atria and the bottom chambers are called ventricles.
Rotherham Hospital use 2 main types of pacemaker:
- single chamber pacemakers - 1 lead that goes into 1 heart chamber
- dual chamber pacemaker - 2 leads that go into 2 chambers of your heart
The type you will have depends on your heart condition.
Are there any alternatives to a pacemaker?
Sometimes changes to your medication can help with a slow heart rhythm.
Some symptoms of an abnormal heart rhythm can be treated using medication but medication may not be as effective as a pacemaker.
What will happen if I decide not to have a pacemaker?
Your doctor may be able to recommend an alternative treatment but you may be at a higher risk of having a cardiac arrest and dying suddenly.
What happens before my pacemaker is fitted?
You will usually be invited to attend Pre-Assessment Clinic in the weeks before your device is fitted.
Please read this information before you attend pre-assessment. You may wish to make a list of questions that you would like to ask.
You will meet the physiologist and nursing staff who will answer any questions you have about the procedure or living with a pacemaker.
It may be useful to bring a friend or relative with you as another person to listen to the information.
Please bring a list of your medications with you.
You may be asked to stop taking anticoagulants (blood thinners), if you are on them, before the procedure. This will be discussed at pre-assessment. You should continue with all other tablets. If there is any possibility that you are pregnant, please inform the medical staff before your procedure.
Having the pacemaker fitted
Your pacemaker will be fitted in the Cardiac Catheter Suite in Rotherham Hospital. On the day of your device implant, you may have a light meal (such as tea and toast) then nothing more to eat or drink until after your procedure.
Please do not bring large sums of money or other valuables into the hospital.
The nurse will insert a cannula (thin tube) into the back of your hand or arm. This is to give you any medications you need during the procedure. You will be given antibiotics via your cannula before the procedure to minimise the chance of infection.
The doctor will explain the procedure in full and you will be asked to sign a consent form. This is to confirm you understand what is involved and agree to proceed.
How will my pacemaker be fitted?
On average the procedure takes around 30 to 60 minutes. You will need to lie flat on an X-ray table. The device will be fitted under local anaesthetic using an X-ray machine. You may also be given a mild sedative to make you feel sleepy and relaxed.
During the procedure you may feel slight pressure and some pushing and pulling below your collarbone. You may also experience some palpitations (feelings of having a fast-beating, fluttering or pounding heart) for a short time.
The doctor guides the lead(s) through a vein below your collarbone and positions them in your heart.
The lead(s) will then be attached to the device. The device is implanted just below your collarbone. The device will be tested during the procedure to ensure it is working well.
Finally, dissolvable stitches are used to seal the wound. These do not need to be removed. You will have a small scar around 3 to 5 centimetres long.
Are there any complications?
The healthcare team will try to reduce the risk of complications.
Any numbers which relate to risk are from studies of people who have had this procedure. Your doctor may be able to tell you if the risk of a complication is higher or lower for you. Some risks are higher if you are older, obese, you are a smoker or have other health problems such as diabetes, heart disease or lung disease.
Some complications can be serious and can even cause death.
The possible complications of inserting a pacemaker are:
- Pain or discomfort where the pacemaker was inserted.
- Bruising where the pacemaker was inserted. This is common and usually fades in about 3 weeks.
- Bleeding after the procedure. It is common to have a little bleeding. Heavy bleeding needing need a blood transfusion or further surgery risk: 1 in 100.
- Pneumothorax, where air escapes into the space around your lung. A pneumothorax is usually small and does not cause any problems. If a lot of air escapes, this can cause a large pneumothorax (risk: less than 1 in 100).
- Blood leaking into the sac that surrounds your heart (cardiac tamponade) (risk: less than 1 in 1,000).
- Developing a blood clot in a vein in your arm (risk: 1 in 50). This does not usually cause any problems but you may need treatment with blood-thinning medication. A blood clot can move through your bloodstream to your lungs (pulmonary embolus), making it difficult for you to breathe.
- Allergic reaction to the equipment, materials or medication.
- Infection of the surgical site (wound) (risk: less than 1 in 200). It is usually safe to shower after 2 days but you should check with the healthcare team. Let the healthcare team know if you get a high temperature, notice pus in your wound, or if your wound becomes red, sore or painful. Your heart specialist may need to remove the pacemaker (risk: less than 1 in 500). A serious infection can be life-threatening.
- The pacemaker developing a fault. The pacemaker may need to be removed (risk: less than 1 in 500). A fault can be life-threatening (risk: less than 1 in 700,000).
- A lead moving out of place (risk: 1 in 50). You may need to have the procedure again to put the lead back in the right position.
- The pacemaker battery showing through your skin. You will need an operation to replace the battery unit (risk: 1 in 400). This is more common in thin people.
- Radiation exposure (the extra risk of developing cancer over a lifetime: on average less than 1 in 3,000 - this is a small increase).
- Electro-magnetic fields interfering with the pacemaker.
You should ask your doctor if there is anything you do not understand.
What happens after the pacemaker is fitted?
After your operation, you will recover in the Cardiac Catheter Suite and will remain there for at least 4 hours, sometimes longer. The nursing staff will check your heart rate, temperature, blood pressure and the amount of oxygen in your blood.
You will usually have a chest X-ray and an ECG (heart tracing). You may also see a Pacing Physiologist, who will test your device using a specialised computer called a programmer.
The programmer communicates with your device and enables the settings to be adjusted to suit your individual needs. This is called a device assessment and is completely painless. Often this assessment is performed whilst you are lying on the X-ray table, so you may be unaware that it has been completed.
You will usually be allowed to go home the same day, unless instructed by the medical team. In some cases the doctor may request that you stay overnight, so we recommend you bring an overnight bag.
Items to bring may include:
- toiletries
- nightwear
- dressing gown
- slippers
- a book or newspaper for while you are waiting
Please do not bring large sums of money or other valuables into the hospital
You will be sent an appointment to attend Device Clinic in approximately 4 to 6 weeks. You will also receive a device Identification Card, which you should carry with you at all times. It contains important information about your pacemaker.
Looking after your wound
Your dressing is waterproof, so you can bath and shower with this dressing still in place. You should remove the dressing after 5 days. At this point you should leave the wound uncovered, unless otherwise instructed by the medical team.
Your stitches are dissolvable, so you do not need to return to have these removed. They usually dissolve within 7 to 10 days.
You should inspect your wound site regularly. Please check for any signs of soreness, inflammation, swelling or leakage. If any of these occur you should contact the Cardiac Device Clinic or your GP as soon as possible. You may need further treatment.
Sometimes, the pacemaker may be visible underneath your skin.
Getting back to normal
After your pacemaker is implanted, you should soon be able to return to your normal activities when you feel ready. Many people find that having a pacemaker improves their quality of life and eliminates symptoms such as dizziness and blackouts.
Your shoulder may feel uncomfortable for a week or so and you may have some bruising and swelling. This usually subsides in 2 to 3 weeks.
It is natural that you may feel worried about having a pacemaker. Some common questions are:
Driving
The DVLA have clear rules about driving. You must not drive for 7 days after your pacemaker is implanted (6 weeks if you have a LGV/PCV group 2 license).
You must inform DVLA that you have a pacemaker:
Drivers Medical Group
DVLA
Swansea
SA99 1TU
Telephone: 0300 790 6806
DVLA website
You will also need to inform you insurance company.
Physical activity
You should take extra care with the arm nearest your pacemaker for the first 4 to 6 weeks (until your first follow up appointment). This is because the leads need time to embed firmly in your heart. After this time it is unlikely that they will move out of position.
For 4 to 6 weeks:
- it is best to avoid reaching up above shoulder height on the side you had your operation. That means not hanging out washing or lifting anything from a high shelf, for example. But it's important to keep your arm mobile by gently moving it to avoid getting a frozen shoulder.
- please do not lift anything over 4.5 kilograms (10 pounds) or put any weight on that arm. You may be asked to wear a sling immediately after your pacemaker is fitted. This is to remind you to be to be careful whilst dressing, washing etc. Please remove the sling after 24 hours.
Some exercise is needed to keep your heart healthy. We advise you to avoid any activities which require strenuous arm movements, such as:
- golf
- squash
- swimming
- contact or rough sports such as rugby and football as the device or leads may become dislodged.
Will electrical equipment stop my pacemaker from working?
All pacemakers have a metal shell to protect them from other electrical signals so you can use most household equipment without any bother.
Ordinary radios, fridges, cookers, televisions, computers and microwaves will not affect your pacemaker as long as they are in good working order. Some specific hand held electrical appliances (such as power tools and base chargers) must be kept at least 15 centimetres (6 inches) away from the pacemaker.
Keep your mobile or cordless phone, Bluetooth device, earbuds or headphones at least 15 centimetres (6 inches) away from your pacemaker.
Ideally hold your phone to the ear opposite to your pacemaker or use loudspeaker so that you can hold it further away.
Travel
If you are travelling through an airport, make sure you tell the security staff that you have a pacemaker so they don’t hold the metal detector over your pacemaker.
Please ensure you carry your identification card and show it to the security staff who may have to search you in another way.
You will also need to make sure your travel insurance company are aware you have a pacemaker fitted.
For more advice speak to a doctor or nurse at your pacemaker clinic.
Shop security systems (also called electronic article surveillance or EAS)
There is a very small risk of interference to your pacemaker, so you are advised to walk through shop doorways at a normal pace.
Don’t linger near an EAS system longer than is necessary.
Be aware that EAS systems are often hidden or camouflaged near the exits for businesses such as retailers.
Don’t lean against the system’s sensors.
Magnets
Do not carry magnets or products containing magnets close to your pacemaker. Avoid contact with large magnets and strong electromagnetic fields, such as:
- car motors - turn off large motors, such as cars or boats, when working on them. They may temporarily 'confuse' your device with the electromagnetic interference created by these large motors
- electronic cigarettes (vapes)
- induction cookers. If you use an induction hob for cooking, keep a distance of at least 60 centimetres (2 feet) from your pacemaker, as this type of hob generates an electromagnetic field that may interfere with your pacemaker settings
- electric arc welding
- amateur radio - under 3 watts should be kept at least 15 centimetres (6 inches) from your pacemaker. 3 to 15 watts should be kept at least 30 centimetres (12 inches) from your pacemaker. 15 to 30 watts should be kept at least 60 centimetres (2 feet) from your pacemaker
- large stereo speakers
- wireless connections
- any device that measures body composition, including fat mass, muscle mass, bone mass, and hydration should not be used by people wearing a pacemaker. This includes scales and smartwatches
- magnetic fasteners such as badges
- a TENS machine for pain relief, and keep electric-pulse body-toning tools below your stomach
- metal detectors
Pacemaker clinic
Your pacemaker will be checked regularly in the pacemaker clinic at Rotherham Hospital. This is a physiologist led clinic and you do not usually see a doctor except in specific circumstances.
During each visit a physiologist will check your device using a special computer known as a programmer.
The physiologist will:
- assess your symptoms and device site
- ensure the pacemaker and leads are working well
- monitor any abnormal rhythms
- assess important information about the battery
- ensure the pacemaker is working well for your individual needs
- offer advice and support
It is very important that you attend your device checks regularly. Following your discharge from hospital after having the device fitted you will be sent an appointment for 4 to 6 weeks for a device check in the clinic. After the initial appointment you will be seen at regular intervals. Most patients are given a remote monitor, this is a small box that you plug in at the side of your bed allowing us to monitor your cardiac device from your home.
Pacemaker clinic is held in the Cardiac Device Suite, A Level.
What happens when the battery runs out?
A pacemaker battery usually lasts between 8 to 10 years. The staff at your pacemaker clinic will keep a close check on the life of your battery and they will not allow it to run out fully.
When the battery is running low, you will need to go back into hospital and have a new pacemaker box fitted.
How to contact us
Pacemaker clinic
01709 424794
Monday to Friday
8:30am to 6pm
Ask to speak to a Pacing Physiologist
Outside of these hours please contact:
Coronary Care Unit (CCU)
01709 424226
Pacemakers - patient information leaflet
Revision due February 2024.
Version: 5.0
©The Rotherham NHS Foundation Trust 2024. All rights reserved.
